Measuring What Matters
Why measure and evaluate your wellness program?
A Harvard Business Review study of 20 companies found an average annual health care cost increase of 1-2% for companies with wellness programs,
compared to the 7% national average.
A detailed evaluation will quickly show you the financial and human benefits of your program as well as areas for improvement. As you complete your evaluation, look back to the goals you set when your organization started its wellness program.
compared to the 7% national average.
A detailed evaluation will quickly show you the financial and human benefits of your program as well as areas for improvement. As you complete your evaluation, look back to the goals you set when your organization started its wellness program.
- Easily leverage your brand, expertise and existing resources to deliver your ideal wellness experience to your population.
- Automate the delivery, administration and management of your wellness program.
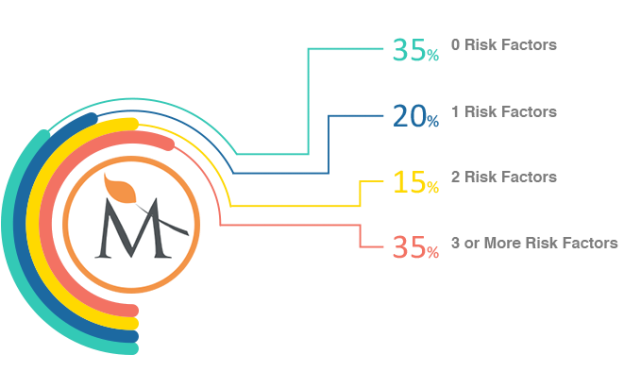
- Guide your population with a personalized user experience based on their specific health profiles and at risk needs.
With Meliora, you have the necessary tools to Measure What Matters.